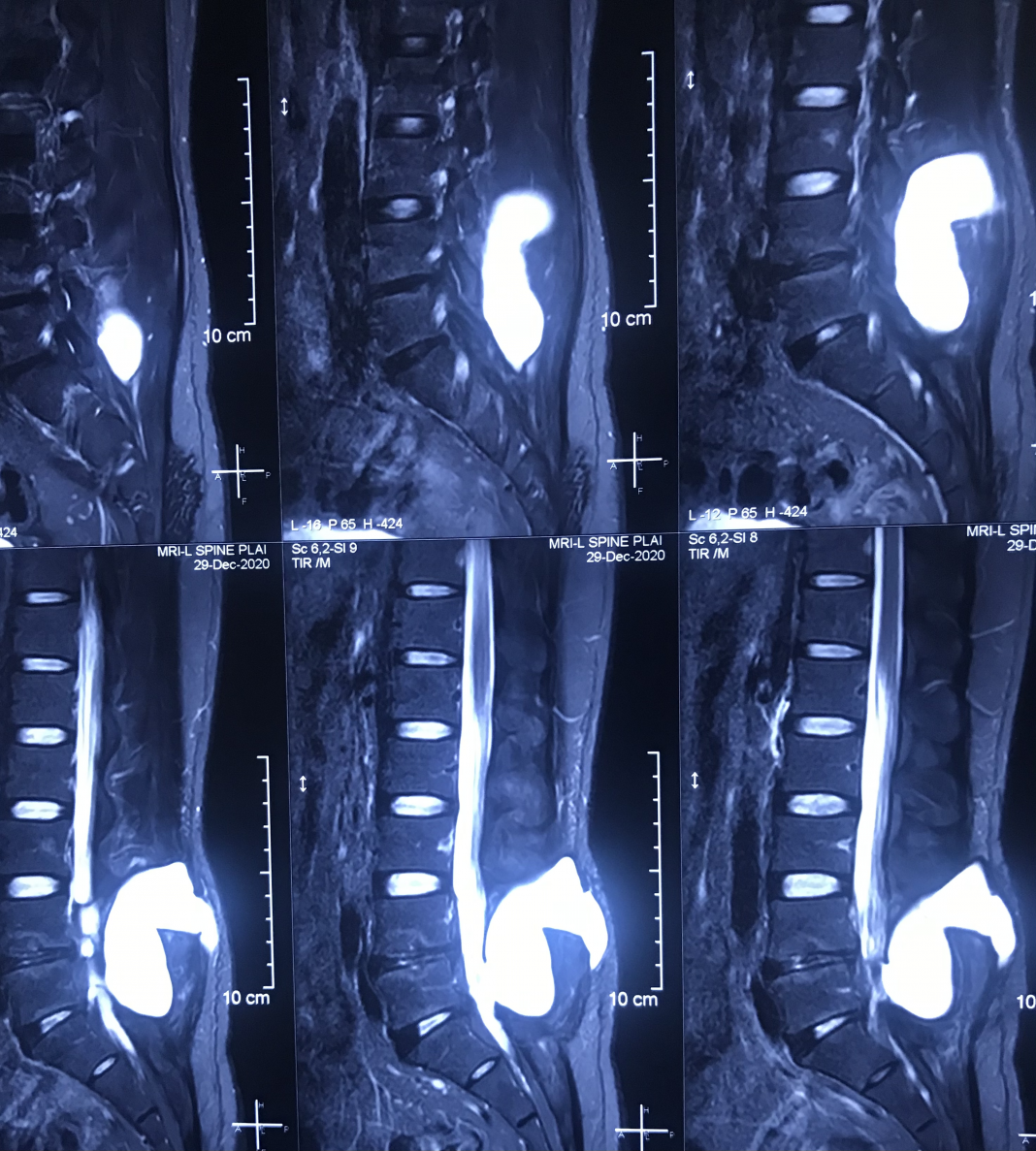
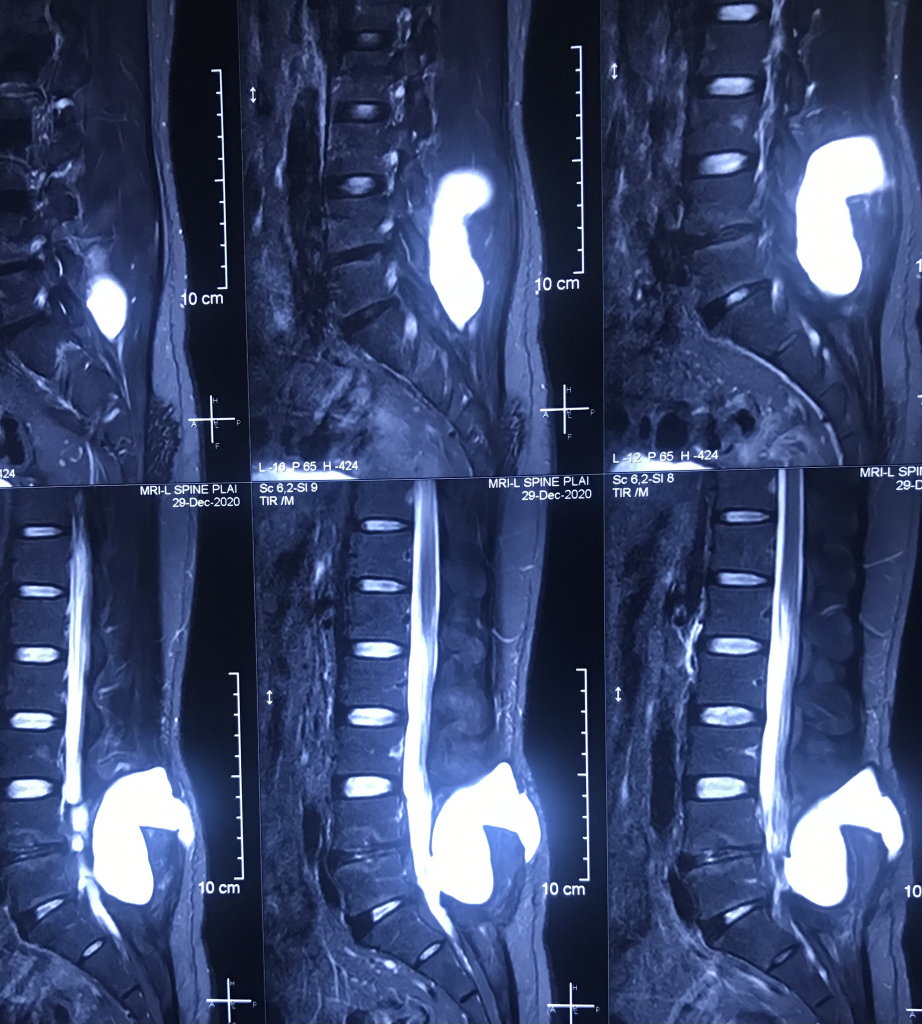
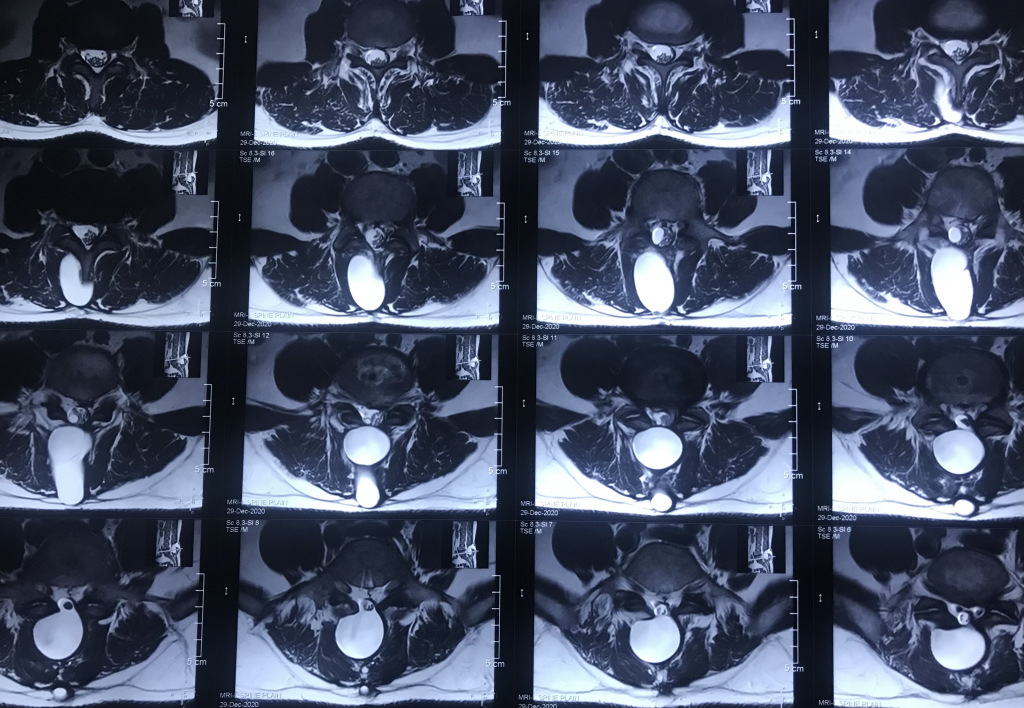
38 Years gentleman, operated for L4-5 disc prolapse 1 year back, now presented with occasional back pain on exertion. Examination does not revealed any significant findings except ?mild bulge over the previous scar.
Postoperative pseudomeningocele was first reported by Hyndman and Gerber in 1946 in a survey of extradural cysts [8]. They classified extradural pseudocysts into two types: iatrogenic and traumatic. The terms “meningocele spurious”, “pseudocyst” or “false cyst”, have also been used to describe pseudomeningoceles [2, 6, 14]. Three types of pseudomeningocele (congenital, iatrogenic and traumatic) were reported by Miller et al. in 1968 [2]. Most pseudomeningoceles are usually associated with neurofibromatosis and Marfan syndrome, and are congenital in origin [1, 3, 8, 15, 16]. Congenital pseudomeningoceles tend to occur in the thoracic or thoracolumbar area [1]. An iatrogenic pseudomeningocele typically occurs as a complication after laminectomy of the lumbar spine [7]. Traumatic pseudomeningoceles are rarest, and are more common in the cervical region (but can also occur in the lumbosacral region after a severe distraction injury) [17, 18]. The incidence of pseudomeningocele after laminectomy ranges from 0.068% (as reported by Swanson et al. in a series of 1,700 laminectomy patients [19]) to 2% (as reported by Teplick et al. in a series of 400 symptomatic post-laminectomy patients [20]).
Postoperative pseudomeningoceles may result from a tear in the dural mater and pia arachnoid that is unnoticed and is left open during surgery [20–23]. If the dural mater and pia arachnoid are torn, CSF extravasates into the paraspinal soft-tissue space. The CSF may be absorbed initially but, after progressive reactions in the connective tissue of the surrounding tissue, CSF is absorbed less readily, resulting in pseudomeningocele formation [2, 5, 14, 20]. More cases of symptomatic, giant pseudomeningoceles developed in the lumbar region (9 out of 11) than other areas (Table 2). This observation is in accordance with other studies [3, 7, 9, 24]. This may be because CSF in the lumbar region is under a higher hydrostatic pressure than that in the cervical spine in the upright posture, and because more surgical procedures are carried out on the lumbar spine [25].
Patients with pseudomeningoceles may present a wide variety of signs and symptoms (though most patients are asymptomatic). Some pseudomeningoceles can be diagnosed based on the fluctuant mass that enlarges with the Valsalva maneuver (e.g., coughing or sneezing) [26]. The common symptoms of postoperative pseudomeningocele are postural headache, localized back pain and radiculopathy. Nerve roots may subsequently herniate through the dural and arachnoid tears, strangulation of the nerve roots within the cyst may lead to radicular pain and motor deficits [12, 23]. Headaches, which are frequently a symptom of large pseudomeningoceles [5], may be the result of a reduction in CSF volume and lowered intracranial pressure [27]. Entrapment of nerve roots in the pseudomeningocele (Figure 3) and pseudomeningocele size seem to be the major factors that determine whether the pseudomeningocele causes symptoms. All of the 11 patients with a giant pseudomeningocele had signs and symptoms (Table 3).
A pseudomeningocele should be considered for patients with recurrent back pain, radicular pain, or a persistent headache after spinal surgery. Most authors consider MRI to be the most effective non-invasive diagnostic tool that can accurately assess the size and location of pseudomeningoceles. MRI was carried out before the combined treatment protocol and was repeated 3 months after surgery to confirm the formation, resolution and recurrence of giant pseudomeningoceles (Figure 2).
The treatment of pseudomeningocele is controversial, particularly in asymptomatic patients. Optimal management of a pseudomeningocele is dependent upon many factors, including sac size, location and symptoms [18]. Small pseudomeningoceles associated with minimal symptoms has been reported to require no treatment [7, 28]. The option of conservative management in asymptomatic patients with a pseudomeningocele was accepted because even large pseudomeningoceles can be seen to “scar down” and resolve over time. Non-surgical management should be the preferred approach if the patient is asymptomatic. Early symptomatic pseudomeningoceles associated with a CSF fistula can be treated with spinal drainage [11]. Symptomatic pseudomeningoceles weeks-to-months after initial surgeries may be treated with surgical dural repair [7, 11, 20]. Aoki reported the treatment of ten patients with postoperative pseudomeningocele by a lumbar shunt [13]. Percutaneous subarachnoid drainage has also been successfully employed to repair dural cutaneous fistulas and early pseudomeningoceles [5]. This procedure can help to create a seal at the leakage site and promote healing by CSF diversion. Primary closure of large dural defects (particularly lateral defects) is difficult. Most authors agree that large dural defects may be closed with patch techniques using autologous tissue, dural allografts, or fibrin glue along the suture line [5, 12, 29]. Removal of pseudomeningoceles and the release of cord or root is required if they adhere to dura.
There are few reports of giant pseudomeningoceles [10]. We reported a combined treatment protocol of open revision surgery for extirpation of pseudomeningoceles, repair of dural tears, and implantation of a subarachnoid catheter for drainage to treat giant pseudomeningoceles. The combined treatment was safe and effective. Surgical complications and recurrence of pseudomeningoceles were not observed at a mean follow-up of 16.5 months (Table 3). Evidence of signs and symptoms indicating a recurrence of pseudomeningocele in these patients was also not observed.
Analyses of the BMI of these patients revealed that being overweight may be a risk factor for the formation of giant pseudomeningoceles after spinal surgery. The mean BMI of the 11 patients was 27.6 kg/m2 (range, 21.0-38.1 kg/m2) (Table 1). For 9 out of the 11 (82%) patients, the BMI was >24.0. Large dural tears with persistent CSF leak, extensive surgical exposure with spinal implants, and revision spinal surgery may also contribute to the formation of giant pseudomeningoceles. Dural tears were identified in all 11 patients at the time of initial surgery that led to subsequent symptomatic pseudomeningocele formation and re-operation. This implied that the initial leaks of CSF were not completely closed even though the entire dural tear had been repaired by primary closure at that time. This emphasizes the importance of adequately training spine surgeons to appropriately address intraoperative CSF leaks. A careful surgical approach is important during revision spinal surgery. Dural tears should be closed first; implantation of a subarachnoid catheter for drainage and repair of soft tissue must be done carefully to prevent a large collection of CSF and constriction of the cauda equina.
Delayed infection of pseudomeningocele was reported by Koo et al. in 1989 [30] and James et al. in 1996 [15]. One of the 11 patients in the present study suffered from CSF infection after the second surgery. This resolved after combining intravenous antibiotics, dural repair with a patch of deep fascia, and placement of a lumbar subarachnoid drain.
Some limitations of the present study must be acknowledged. Comparisons among different treatments such as conservative management, epidural blood patch, subarachnoid drainage alone, and surgery for giant pseudomeningoceles should be obtained. Indications of open surgery dependent upon pseudomeningocele size should also be carried out. Long-term follow-up studies are warranted to determine if the combined treatment protocol is an effective and safe procedure.
Conclusions
A combined treatment protocol involving open revision surgery for extirpation of the pseudomeningocele, repair of dural tears, and implantation of a subarachnoid catheter for drainage is safe and effective to treat giant pseudomeningoceles.
References
- 1.Sutterlin CE, Grogan DP, Ogden JA: Diagnosis of developmental pathology of the neuraxis by magnetic resonance imaging. J Pediatr Orthop. 1987, 7: 291-297.CAS Article PubMed Google Scholar
- 2.Miller PR, Elder FW: Meningeal pseudocysts (meningocele spurius) following laminectomy. Report of ten cases. J Bone Joint Surg Am. 1968, 50: 268-276.CAS PubMed Google Scholar
- 3.Wilkinson HA: Nerve-root entrapment in “traumatic” extradural arachnoid cyst. J Bone Joint Surg Am. 1971, 53: 163-166.CAS PubMed Google Scholar
- 4.Barron JT: Radiologic case study. Lumbar pseudomeningocele. Orthopedics. 1990, 13: 608-609.Google Scholar
- 5.Pau A: Postoperative “meningocele spurius”. Report of two cases. J Neurosurg Sci. 1974, 18: 150-152.CAS PubMed Google Scholar
- 6.Cook DA, Heiner JP, Breed AL: Pseudomeningocele following spinal fracture. A case report and review of the literature. Clin Orthop Relat Res. 1989, 247: 74-79.PubMed Google Scholar
- 7.Lee KS, Hardy IM: Postlaminectomy lumbar pseudomeningocele: report of four cases. Neurosurgery. 1992, 30: 111-114.CAS Article PubMed Google Scholar
- 8.Hyndman OR, Gerber WF: Spinal extradural cysts, congenital and acquired: report of cases. J Neurosurg. 1946, 3: 474-486. 10.3171/jns.1946.3.6.0474.CAS Article PubMed Google Scholar
- 9.O’Connor D, Maskery N, Griffiths WE: Pseudomeningocele nerve root entrapment after lumbar discectomy. Spine. 1998, 23: 1501-1502. 10.1097/00007632-199807010-00014.Article PubMed Google Scholar
- 10.Hader WJ, Fairholm D: Giant intraspinal pseudomeningoceles cause delayed neurological dysfunction after brachial plexus injury: report of three cases. Neurosurgery. 2000, 46: 1245-1249. 10.1097/00006123-200005000-00044.CAS Article PubMed Google Scholar
- 11.McCormack BM, Zide BM, Kalfas IH: Cerebrospinal fluid fistula and pseudomeningocele after spine surgery. Spine Surgery, techniques, complication avoidance and management. Edited by: Edward C, Benzel EC. 2005, 2: 2033-2042.Google Scholar
- 12.Hadani M, Findler G, Knoler N, Tadmor R, Sahar A, Shacked I: Entrapped lumbar nerve root in pseudomeningocele after laminectomy: report of three cases. Neurosurgery. 1986, 19: 405-407. 10.1097/00006123-198609000-00012.CAS Article PubMed Google Scholar
- 13.Aoki N: Lumboperitoneal shunt for the treatment of postoperative persistent collection of subcutaneous cerebrospinal fluid (pseudomeningocele). Acta Neurochir (Wien). 1989, 98: 32-34. 10.1007/BF01407173.CAS Article Google Scholar
- 14.Pagni CA, Cassinari V, Bernasconi V: Meningocele spurius following hemilaminectomy in a case of lumbar discal hernia. J Neurosurg. 1961, 18: 709-710. 10.3171/jns.1961.18.5.0709.CAS Article PubMed Google Scholar
- 15.Dastur HM: The radiological appearances of spinal extradural arachnoid cysts. J Neurol Neurosurg Psychiatry. 1963, 26: 231-235. 10.1136/jnnp.26.3.231.CAS Article PubMed PubMed Central Google Scholar
- 16.Maiuri F, Corriero G, Giampaglia F, Simonetti L: Lateral thoracic meningocele. Surg Neurol. 1986, 26: 409-412. 10.1016/0090-3019(86)90147-3.CAS Article PubMed Google Scholar
- 17.Kolawole TM, Patel PJ, Naim R: Post-surgical anterior pseudomeningocele presenting as an abdominal mass. Comput Radiol. 1987, 11: 237-240. 10.1016/0730-4862(87)90004-7.CAS Article PubMed Google Scholar
- 18.Nairus JG, Richman JD, Douglas RA: Retroperitoneal pseudomeningocele complicated by meningitis following a lumbar burst fracture. Spine. 1996, 21: 1090-1093. 10.1097/00007632-199605010-00020.CAS Article PubMed Google Scholar
- 19.Swanson HS, Fincher EF: Extradural arachnoidal cysts of traumatic origin. J Neurosurg. 1947, 4: 530-538. 10.3171/jns.1947.4.6.0530.CAS Article PubMed Google Scholar
- 20.Teplick JG, Peyster RG, Teplick SK, Goodman LR, Haskin ME: CT Identification of postlaminectomy pseudomeningocele. AJR Am J Roentgenol. 1983, 140: 1203-1206.CAS Article PubMed Google Scholar
- 21.Winkler H, Powers JA: Meningocele following hemilaminectomy; report of 2 cases. N C Med J. 1950, 11: 292-294.CAS PubMed Google Scholar
- 22.Rinaldi I, Peach WF: Postoperative lumbar meningocele. Report of two cases. J Neurosurg. 1969, 30: 504-507. 10.3171/jns.1969.30.4.0504.CAS Article PubMed Google Scholar
- 23.Rinaldi I, Hodges TO: Iatrogenic lumbar meningocoele: report of three cases. J Neurol Neurosurg Psychiatry. 1970, 33: 484-492. 10.1136/jnnp.33.4.484.CAS Article PubMed PubMed Central Google Scholar
- 24.Inci S, Akbay A, Bertan V: Postoperative lumbar pseudomeningocele. Turkish Neurosurgery. 1994, 4: 44-46.Google Scholar
- 25.Hawk MW, Kim KD: Review of spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus. 2000, 9: e5-10.3171/foc.2000.9.1.5.CAS Article PubMed Google Scholar
- 26.Rocca A, Turtas S, Pirisi A, Agnetti V: Iatrogenic lumbar pseudomeningocele. Zentralbl Neurochir. 1986, 47: 311-315.CAS PubMed Google Scholar
- 27.Couture D, Branch CL: Spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus. 2003, 15: E6-10.3171/foc.2003.15.6.6.Article PubMed Google Scholar
- 28.Hadley MN, Carter LP: Sacral fracture with pseudomeningocele and cerebrospinal fluid fistula: case report and review of the literature. Neurosurgery. 1985, 16: 843-846.CAS Article PubMed Google Scholar
- 29.Shaffrey CI, Spotnitz WD, Shaffrey ME, Jane JA: Neurosurgical applications of fibrin glue: augmentation of dural closure in 134 patients. Neurosurgery. 1990, 26: 207-210. 10.1097/00006123-199002000-00004.CAS Article PubMed Google Scholar
- 30.Koo J, Adamson R, Wagner FC, Hrdy DB: A new cause of chronic meningitis: infected lumbar pseudomeningocele. Am J Med. 1989, 86: 103-104. 10.1016/0002-9343(89)90238-6.CAS Article PubMed Google Scholar